All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MDS Alliance.
The mds Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mds Hub cannot guarantee the accuracy of translated content. The mds and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MDS content recommended for you
MDS/MPN: Diagnostic differences between WHO 5th edition and ICC schemes
Do you know... Diagnostic discrepancies between the new World Health Organization (WHO) 5th edition and International Consensus Classification (ICC) schemes for the diagnosis of MDS and MPN may cause challenges for both physicians and patients. Which one of the following statements is true?
The recent revision of the World Health Organization (WHO) classification of myeloid neoplasms 4th edition has generated two separate classification schemes for the diagnosis of myelodysplastic syndromes (MDS) and myeloproliferative neoplasms (MPN); the International Consensus Classification (ICC) and the WHO classification 5th edition both provide valuable diagnostic guidance for healthcare professionals; however, diagnostic discordance may arise from the application of different classification models.
Recently, Benton et al.1 published a report in Journal of Clinical Pathology reviewing 64 patients diagnosed with MPN/MDS using both schemes and assessing diagnostic inconsistencies to highlight significant differences between the models. Here, we highlight the key findings in the article.
Methods
- All patient cases were collected between January 2016 and September 2022, and all patients underwent a bone marrow biopsy.
- Diagnostic interpretation was performed by three board-certified hematologists.
- Only patients with a first-time of MDS/MPN were included.
- Any patients with a pre-existing diagnosis were excluded from evaluation.
- All patient diagnoses and classifications were based initially on the WHO classification of myeloid neoplasms 4th edition.
- Each case was subsequently recategorized using both new schemes.
- A complete consensus was required from all three hematologists.
- Two categories of difference were formed:
- ‘significant differences’, defined as changes in diagnostic category, a change in treatment, and/or whether clinical trial eligibility was impacted; and
- ‘nominal/nomenclature-related differences’, defined as word order changes with no impact on diagnostic category, treatment approach, or clinical trial eligibility.
Results
- A total of 64 patient cases were included in the review
- Nine cases were identified to have nominal diagnostic differences (Figure 1)
- One case was identified to have a significant diagnostic difference (Figure 2)
Figure 1. Patient cases with nominal diagnostic differences*
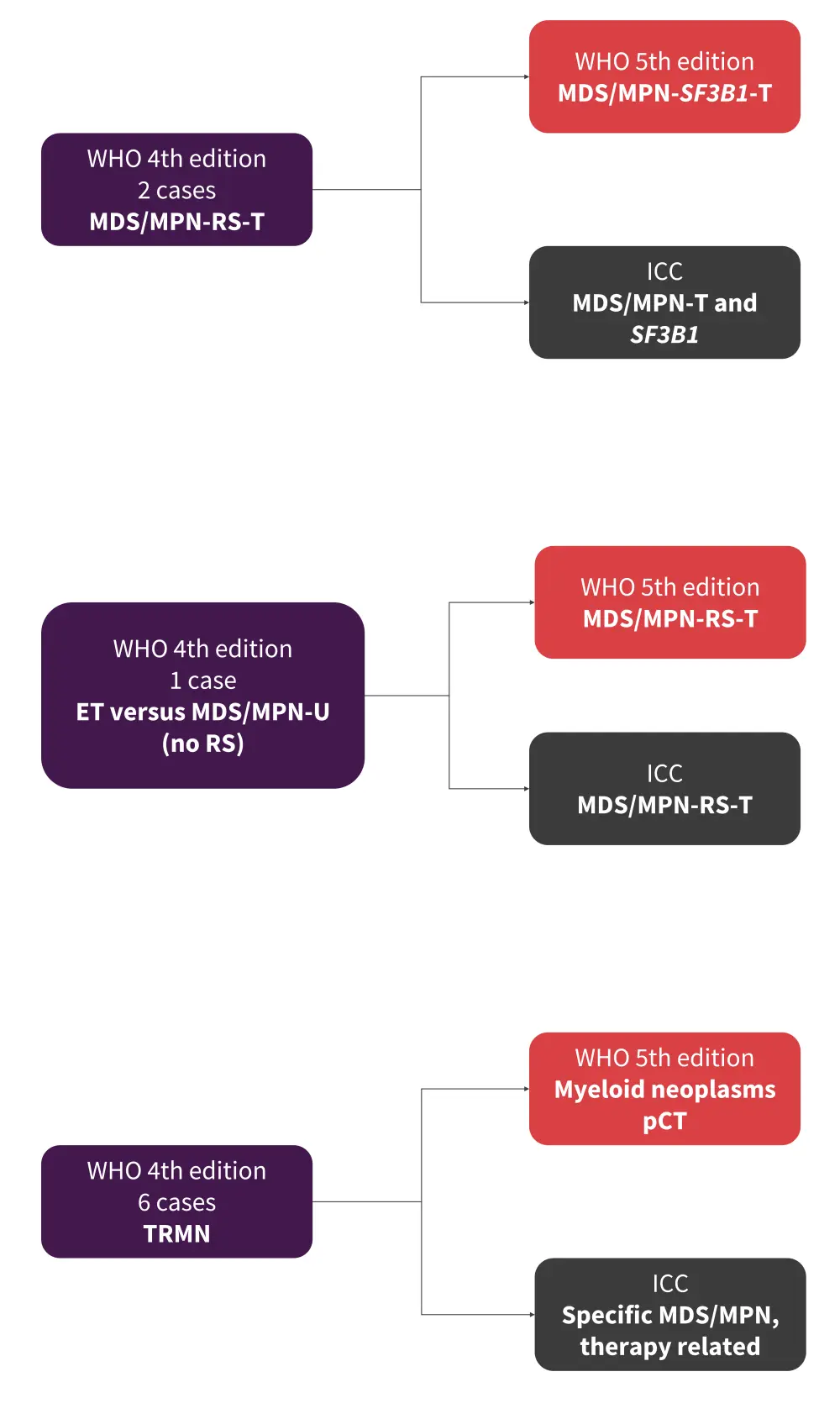
ET, essential thrombocythemia; ICC, International Consensus Classification; MDS, myelodysplastic syndrome; MPN, myeloproliferative neoplasm; pCT, post cytotoxic therapy; RS, ringed sideroblasts; T, thrombocytosis; TRMN, treatment-related myeloid neoplasm; U, unclassifiable; WHO, World Health Organization.
*Adapted from Benton, et al.1
Figure 2. Patient case with a significant diagnostic difference*
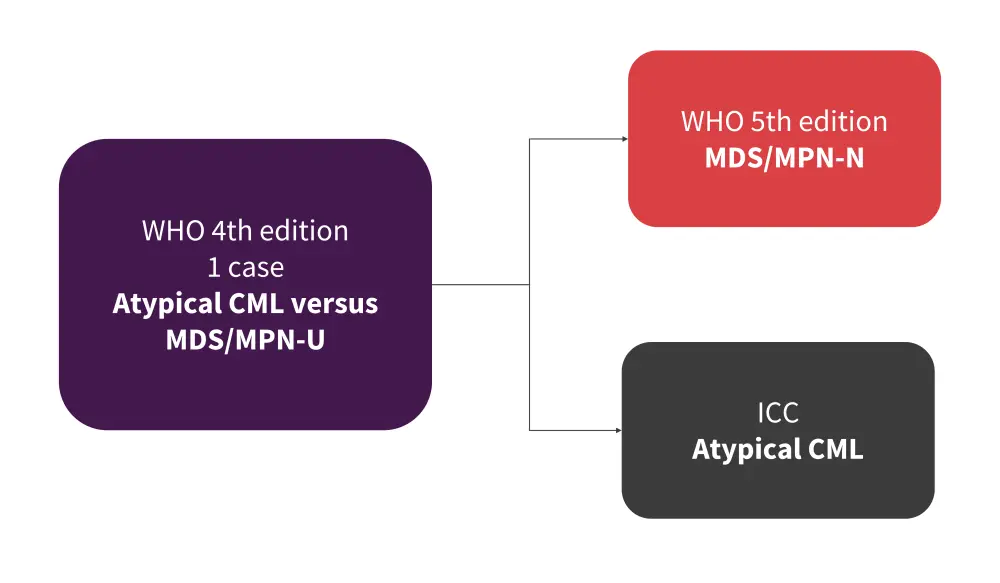
CML, chronic myeloid leukemia; ICC, International Consensus Classification; MDS, myelodysplastic syndrome; MPN, myeloproliferative neoplasm; N, neutrophilia; U, unclassifiable; WHO, World Health Organization.
*Adapted from Benton, et al.1
- Significant diagnostic discrepancies were identified in 84% of patient cases when comparing the WHO 4th edition with both new 2022 classifications.
What does this mean for current diagnostic practices?
- For the 9 patients deemed to have nominal diagnostic differences, the information given by each classification was almost identical.
- However, simple word order changes could present as a challenge for individuals inexperienced with the new classifications.
- These differences have the potential to impact practice and care through increased patient confusion and physician workload, as well as altering future clinical trials.
- The single case deemed to have significant differences between the two classifications had the potential to cause notable confusion.
- Fortunately, there was no implication for treatment approach in this case, due to the lack of standard therapies for these rare conditions.
- In contrast, when comparing the WHO 4th edition to the new classifications there was frequent diagnostic movement.
- Most changes were deemed significant.
- Several cases diagnosed as MDS in the WHO 4th edition would now be classified as chronic myelomonocytic leukemia.
- There are also potential challenges surrounding the separation of MDS/ MPN in accelerated-/blast-phase versus acute myeloid leukemia (AML).
- Confusion in the separation of MDS/MPN versus MDS with leukocytosis, monocytosis, or thrombocytosis may arise.
- Both distinctions remain very difficult to identify, and currently only a prior history of MPN/MDS is able to separate the entities.
- Both updated classifications are based heavily on genetic data, yet mutation analysis by next-generation sequencing is often unavailable or delayed.
- Several other uncovered gaps between the two new schemes include cases with overlapping features and diagnostic grey areas.
- The TP53 mutation has become increasingly significant in the new classifications.
- However, the mutation is uncommon in MDS/MPN, and there is no guidance on the significance of biallelic TP53 mutations in this set of patients.
Conclusion
Although not immediately clinically significant, the diagnostic discrepancies highlighted have the potential to increase physician workload and cause unnecessary confusion for healthcare professionals and patients alike. There is potential for long-term challenges to arise which will impact on clinical trial eligibility and treatment disparities. Resolution of these issues is important to avoid confusion and ensure standardized practices, enabling optimal patient outcomes.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

