All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MDS Alliance.
The mds Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mds Hub cannot guarantee the accuracy of translated content. The mds and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MDS content recommended for you
Real-world transfusion practices and experiences for patients diagnosed with MDS
Do you know... Patients recommended several improvements to their transfusion experience. Out of the following four recommendations suggested by patients, which one was the most popular?
Of patients who are diagnosed with myelodysplastic syndromes (MDS), 80–85% experience anemia, and 50% of these require red blood cell transfusions.1 It is well understood that anemia and transfusion-dependence have a significant impact on the quality of life of patients and are associated with poorer survival.
Currently, there is limited data on real world transfusion practices. As a result, Vijenthira, et al.1 conducted a multinational audit of real-world transfusion practices to better understand patient experiences and preferences. We summarize the findings below.
Study design
A web-based cross-sectional survey was produced by a panel of experts, with a total of 57 questions in both multiple choice and open-ended question formats. Patients with MDS in the US, UK, and Canada were surveyed and included if they were transfusion-dependent and if they had received at least one unit of red blood cells in the 8 weeks before the survey completion.
The data collected included demographic information and transfusion history, measures of subjective experience, healthcare utilization, economic impact, and patient opinions on how to improve their experience.
Results
A total of 447 eligible patients took part in the survey between August 2017 and January 2018; of these, 344 were complete submissions. The median age of the eligible patient cohort was 72 years and most patients had lived with MDS for 3 years. The patient characteristics are shown in Table 1.
Table 1. Baseline characteristics of patients according to country of origin*
|
MDS, myelodysplastic syndromes. |
||||
|
Characteristic, % (unless otherwise stated) |
US |
Canada |
UK |
Total |
|---|---|---|---|---|
|
Median age, years |
73 |
73 |
69 |
72 |
|
Sex |
|
|
|
|
|
Female |
43 |
44 |
55 |
45 |
|
Years with diagnosis |
3 |
3 |
3 |
3 |
|
MDS risk category |
|
|
|
|
|
Low |
42 |
57 |
57 |
45 |
|
High |
27 |
22 |
18 |
27 |
|
Do not know |
29 |
22 |
25 |
28 |
|
Cytogenetic risk category |
|
|
|
|
|
Low or intermediate |
20 |
0 |
31 |
18 |
|
Poor |
9 |
9 |
8 |
9 |
|
Do not know |
71 |
91 |
62 |
73 |
|
When did transfusion dependence occur? |
|
|
|
|
|
At diagnosis |
32 |
39 |
47 |
35 |
|
≤6 months after diagnosis |
16 |
15 |
20 |
17 |
|
7–12 months |
12 |
7 |
14 |
11 |
|
>12 months after diagnosis |
40 |
39 |
20 |
37 |
Out of the eligible patients, 35% had received red blood cell transfusions at diagnosis compared with 17% who received transfusions ≤6 months after diagnosis, followed by 11% of patients who received transfusions 7–12 months after diagnosis. The median number of units that patients received in a single visit was two, with 50% of patients having visited an outpatient center >2 times within a 4‑week period. Most patients knew their hemoglobin threshold for transfusion, the most common being <80 g/L, which was identified in 76% of patients. Most transfusions were organized the same day or administered within 1–2 days after patients reached their hemoglobin threshold. A total of 83 patients experienced an adverse effect during the transfusion process, with 57% reporting iron overload and 32% reporting a minor allergic reaction.
Quality of life
Patients listed several concerns before transfusion, including adverse effects and the safety of the blood supply. The most common are shown in Figure 1.
Figure 1. Patient concerns prior to transfusion*
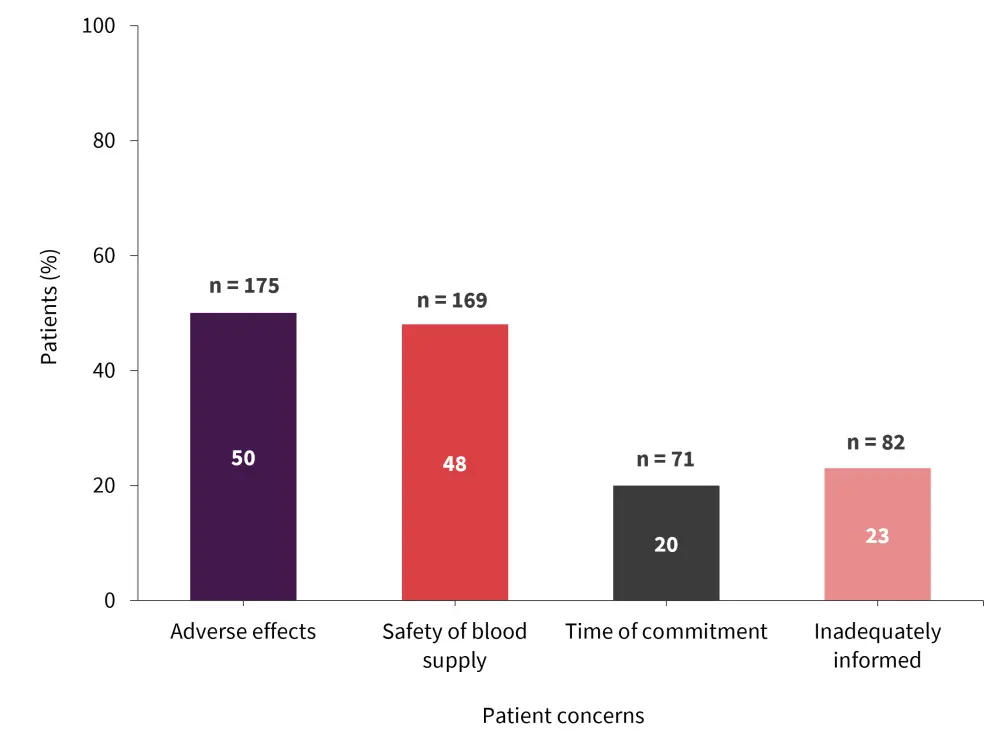
*Adapted from Vijenthira, et al.1
Before receiving red blood cell transfusions, patients reported a range of common symptoms (Figure 2). The symptoms with the largest impact on a patient’s quality of life were fatigue, reported by 46% of patients, and shortness of breath, reported by 24% of patients. A total of 297 patients felt it took at least 1 day after transfusion to feel symptomatic relief (Figure 3). Furthermore, 65% of patients reported symptom relief for at least 5 days and only 20% reported feeling worse 1–2 days after the transfusion had been administered.
Figure 2. Common symptoms experienced before transfusion*
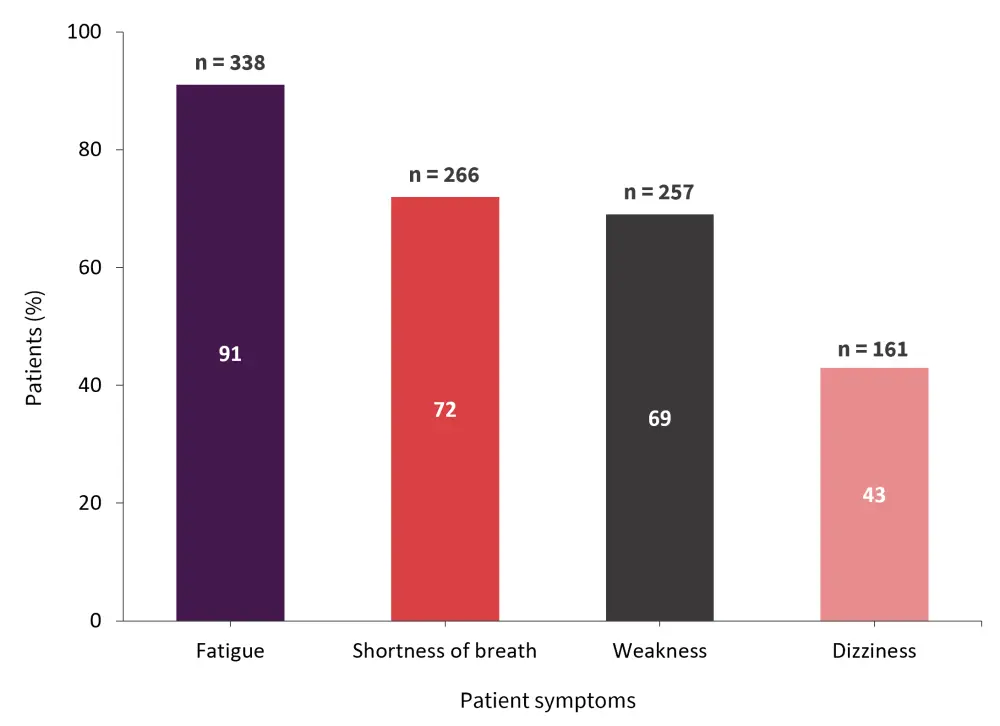
*Adapted from Vijenthira, et al.1
A total of 213 patients reported travelling for <30 minutes to reach their chosen outpatient center and a further 116 reported travelling between 30 minutes to 1 hour. Interestingly, 19% of patients felt that their travel time to the clinic negatively impacted their quality of life. Patients were also asked about their average length of visit; 66% spent 4 hours or longer and 6% reported staying for over 7 hours. Not all patients had access to a local outpatient center; 19% reported having to travel to an emergency department in order to receive their transfusion. Moreover, patients spent an average of $20 USD per month in relation to their transfusions, with 31% reporting economic hardship. There was no significant difference in the average amount of money spent per month between countries (p = 0.7).
Patients had several recommendations to improve the transfusion experience (Figure 3). In total, 51% of patients said they would prefer same-day cross-match and transfusion. When asked about the frequency of transfusions, 45% of patients either strongly agreed or agreed that a reduction in frequency would increase their quality of life. The ability to check blood counts at home was listed by 74% of patients as another potential improvement and 26% of patients also asked for a higher transfusion threshold.
Lastly, with regards to a preferred threshold, 62% of patients listed <85 g/L, followed by 20% of patients listing <100 g/L as their preferred value.
Figure 3. Patient recommendations to improve the transfusion experience*
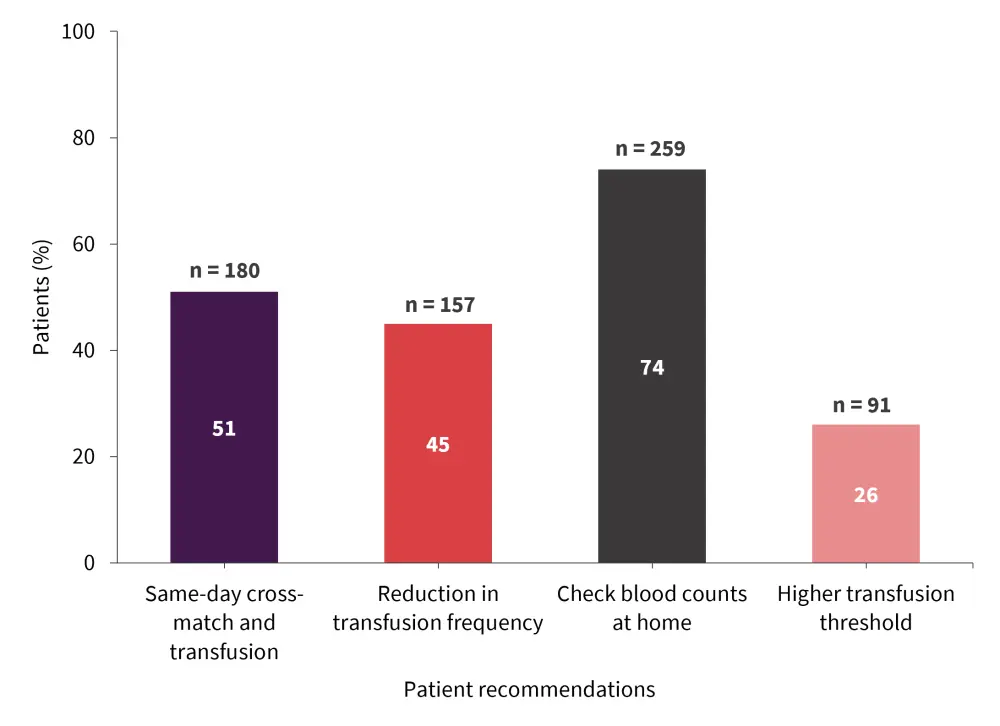
*Adapted from Vijenthira, et al.1
Conclusion
While transfusion is often essential for patients diagnosed with MDS, it has a significant impact on the overall survival and quality of life of the patient. The responses gathered in the study by Vijenthira, et al. highlight areas of potential further investigation to improve patient experience. These include methods for a more efficient transfusion process and more individualized hemoglobin thresholds.
While the study gathered information on patient experiences, there were several limitations. Due to the survey being sent through mailing lists, selection bias was present. Furthermore, this format of gathering information excludes those without or who cannot use a computer, as well as those who do not speak English. Moreover, the majority of patients were White and from the US, and so the authors may not have completely understood the experiences of all races and nationalities. Since it is a cross-sectional survey, recall bias may also have been a problem. The study did not provide a longitudinal view of patient experience over time and did not include methods to validate the patient’s self-reported World Health Organization (WHO) subtype or International Prognostic Scoring System (IPSS) scores with clinical data. Finally, there was potential for patients to incorrectly recall details about their recent care; therefore, misclassification bias may have occurred.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

