All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MDS Alliance.
The mds Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mds Hub cannot guarantee the accuracy of translated content. The mds and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MDS content recommended for you
Improvement in QoL post red cell transfusion and feasibility of peri-transfusion QoL assessment in patients with MDS
Myelodysplastic syndromes (MDS) are a heterogenous group of bone marrow disorders characterized by abnormal blood cell development, cytopenias, and risk of developing acute myeloid leukemia (AML). Symptomatic anemia in patients with MDS is treated with red cell transfusions to improve both the symptoms of anemia and the quality of life (QoL) of patients, though the impact on QoL has yet to be clearly demonstrated. Previous studies have reported variable results using generic QoL assessment tools, and evidence regarding the threshold hemoglobin (Hb) level for red cell transfusion in patients with MDS was conflicted. Recently, however, Abel and colleagues1 developed and validated the Quality of Life in Myelodysplasia Scale (QUALMS), a QoL scale specific to patients with MDS, and an expert consensus was reached stating that a Hb level of 7.5 g/dl is the lowest level at which it is considered safe to waive transfusion in patients with MDS.
Recently, Abel et al.2 published a study in Transfusion reporting on whether QoL improved post-transfusion and whether peri-transfusion QoL assessments (PTQA) could help guide future transfusion decisions. Here we summarize the key findings.
Study design
This was a prospective, multicenter pilot study of adult patients with confirmed MDS and Hb level ≥ 7.5 g/dl. Eligible patients underwent PTQA, and MDS-related QoL was assessed using QUALMS 1 day before and 7 days after red cell transfusion. Thirty-three items were measured with QUALMS and scored from 0 to 100, where a higher score was associated with better QoL. A change in the QUALMS score of 5 or more points was considered clinically significant.
- A follow-up questionnaire including questions about decisional regret, perceptions of care, and perceived stress at 8 weeks of post-index transfusion was administered to enrolled patients, and an exploratory analysis was performed.
- Patients who completed PTQA were matched to historical cohorts in a further analysis to investigate any differences in red cell utilization in the 8 weeks after the index transfusion.
Results
A total of 61% (38/62) of enrolled patients completed the pre- and post-transfusion QUALMS. One post-questionnaire was received but lost and 24 patients did not complete PTQA (Table 1), mostly due to their Hb level being below 7.5 g/dl at the time of PTQA index transfusion. Consequently, a total of 37 patients were available for pre-/post-analyses.
Table 1. Enrolled patients not completing PTQA*
|
AML, acute myeloid leukemia; PTQA, peri-transfusion QoL assessment. |
|
|
Reason for not completing PTQA, % |
n = 24 |
|---|---|
|
Later become ineligible or lost to follow-up |
44 |
|
Died before index transfusion |
16 |
|
Transplanted before index transfusion |
16 |
|
Progressed to AML before index transfusion |
8 |
|
Did not need a transfusion after enrolling |
8 |
|
Withdrew consent |
4 |
Exploratory analyses
- The mean age of patients who underwent PTQA was 73 years and 42% of patients were female (Table 2).
- The mean pre-transfusion QUALMS score was 57 in the 37 patients analyzed compared with 67 in the 2016 QUALMS validation study, which had 255 patients.1
- Clinically significant increase in QoL score after transfusion was observed in 35% of patients (95% CI, 22−51) (Figure 1) with a mean increase of 14 points (standard deviation [SD] = 5). In patients with a decrease in QOL score, the mean decrease was 7 points (SD = 2).
- The greatest change in score was seen for items assessing physical burden, including low energy and shortness of breath.
Table 2. Descriptive statistics for the evaluable cohort*
|
CI, confidence interval; ECOG, Eastern Cooperative Oncology Group; IPSS-R, Revised International Prognostic Scoring System; QUALMS, Quality of life in Myelodysplasia Scale; RBC, red blood cell; SD, standard deviation. |
|
|
Characteristic |
Evaluable cohort |
|---|---|
|
Mean age (SD) |
73 (11.6) |
|
Transfusion-dependent, % |
89.5 |
|
ECOG, % |
|
|
0 |
22.2 |
|
1 |
58.3 |
|
2 |
19.4 |
|
Mean IPSS-R score (SD) |
4.19 (2.2) |
|
Median days from diagnosis to index transfusion |
209 |
|
Mean index transfusion hemoglobin (SD) |
8.05 (0.6) |
|
Median index RBC units received |
1 |
|
Mean QUALMS score (SD) |
|
|
Pre-transfusion |
56.5 (14.5) |
|
Post-transfusion |
59.9 (17.9) |
|
Change in QUALMS score, % (95% CI) |
|
|
Increase (up to 5 points or more) |
35.1 (22−51) |
|
No change (within 4.9 points up or down) |
45.9 (31−62) |
|
Decrease (down 5 points or more) |
18.9 (9−34) |
Figure 1. Change in the QUALMS score 7 days post-transfusion*
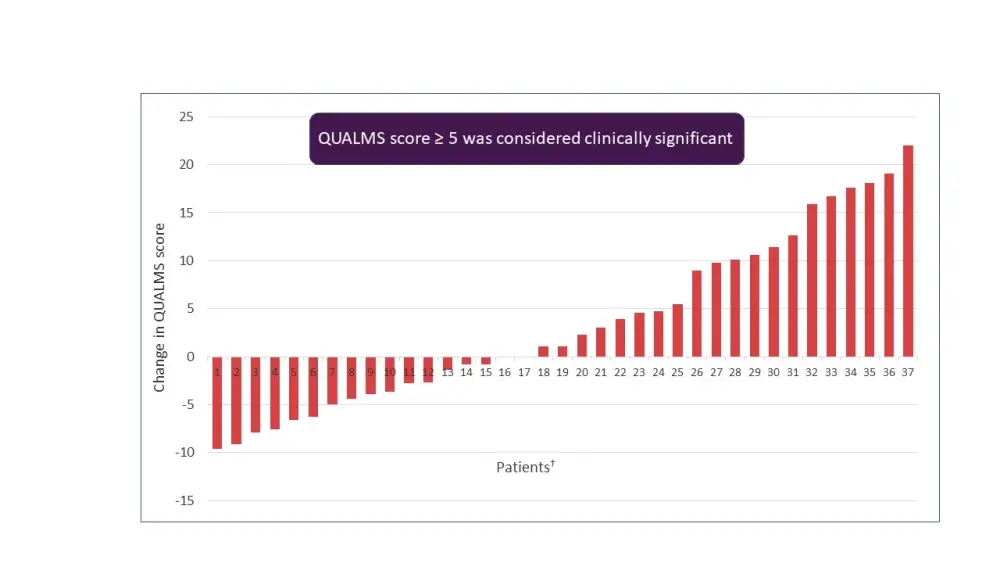
*Adapted from Abel et al.2
†Each bar represents one patient.
- Six of the 38 patients who completed PTQA did not complete the follow-up survey and one died; of the remaining 31 patients, 55% thought subsequent transfusion was the right decision while 9% of patients regretted their decision.
- 23% of patients reported discussing PTQA results with their provider, and of these, three patients reported that the PTQA results affected their decision to pursue further red cell transfusions.
Further analyses
Twenty-five patients were matched with controls, and the use of red cell units in the 8-week follow-up period was higher in the PTQA group compared with the control group (p = 0.03) with a median difference of 2.5 (95% CI, 0−5) in the units of red cells received.
Conclusion
The exploratory analysis demonstrated that only one-third of patients with MDS may have an improved QoL as measured by QUALMS after red cell transfusion. These findings are suggestive of potential risks and costs associated with red cell transfusions without achieving QoL improvements in patients with MDS. The study also demonstrated the feasibility of the PTQA approach that may help in informed shared decision-making regarding red cell transfusion. However, the findings from the study warrant further qualitative research on how PTQA data can be better utilized in outpatient clinics.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

