All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MDS Alliance.
The mds Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mds Hub cannot guarantee the accuracy of translated content. The mds and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MDS content recommended for you
Peri-transfusion quality-of-life assessment to help future transfusion decisions for patients with MDS
Anemia-related fatigue in myelodysplastic syndromes (MDS) can lead to dependance on red blood cell (RBC) transfusions and a reduced quality of life. Indeed, a retrospective multicenter study performed across France by the Francophone Myelodysplasia Group (Groupe Francophone des Myélodysplasies), analyzing 100 patients with MDS over a 6-month period, highlighted that 79% of patients had a high transfusion burden.1 Of these patients, 22% required inpatient hospitalization, with 36% of them requiring emergency RBC transfusion due to symptomatic anemia; the median total transfusion cost for each patient, during the 6-month period, was €16,188.1
At the European School of Haematology (ESH) 8th Translational Research Conference: Myelodysplastic Syndromes, Gregory A. Abel2 discussed the potential applications of a peri-transfusion quality-of-life assessment to help future transfusion decisions. He reported the workflow used to define the minimum hemoglobin level required in patients who undergo stem cell transplantation (SCT), as well as the overall feasibility of the assessment process.2 We summarize the findings below.
Minimum hemoglobin level to undergo stem cell transplantation
Study design
A panel of 13 expert physicians were brought together, which included 12 MDS experts and one transfusion medicine expert, to decide on the accepted hemoglobin threshold required to undergo RBC transfusion. A modified Delphi technique, incorporating elements from the RAND/UCLA Appropriateness Method, was used during multiple rounds of assessment, anonymous presentations of results, and discussions. The end goal was to reach a pre-specified consensus of 75%.
Results
The study consisted of three rounds of assessments by the panel:
- Round 1
- The majority of participants (7/13; 54%) agreed on a hemoglobin level of 7 g/dL
- A threshold no greater than 8 g/dL was agreed by nearly all (12/13; 92%)
- Round 2 (narrowed answers based on results from Round 1)
- Majority (7/13; 54%) agreed on a hemoglobin level of 7.5 g/dL
- A threshold no greater than either 7 g/dL or 7.5 g/dL was agreed by nearly all (12/13; 92%)
- Round 3
- Majority (8/13; 62%) agreed on a hemoglobin level of 7.5 g/dL
- Panel was unable to reach a pre-met consensus for a specific threshold
- There was a 100% consensus of a threshold no greater than 7.5 g/dL
Results from the assessments are shown in Figure 1.
Figure 1. Hemoglobin level threshold for transfusion assessment accepted by the expert panel: A Round 1; B Round 2; C Round 3*
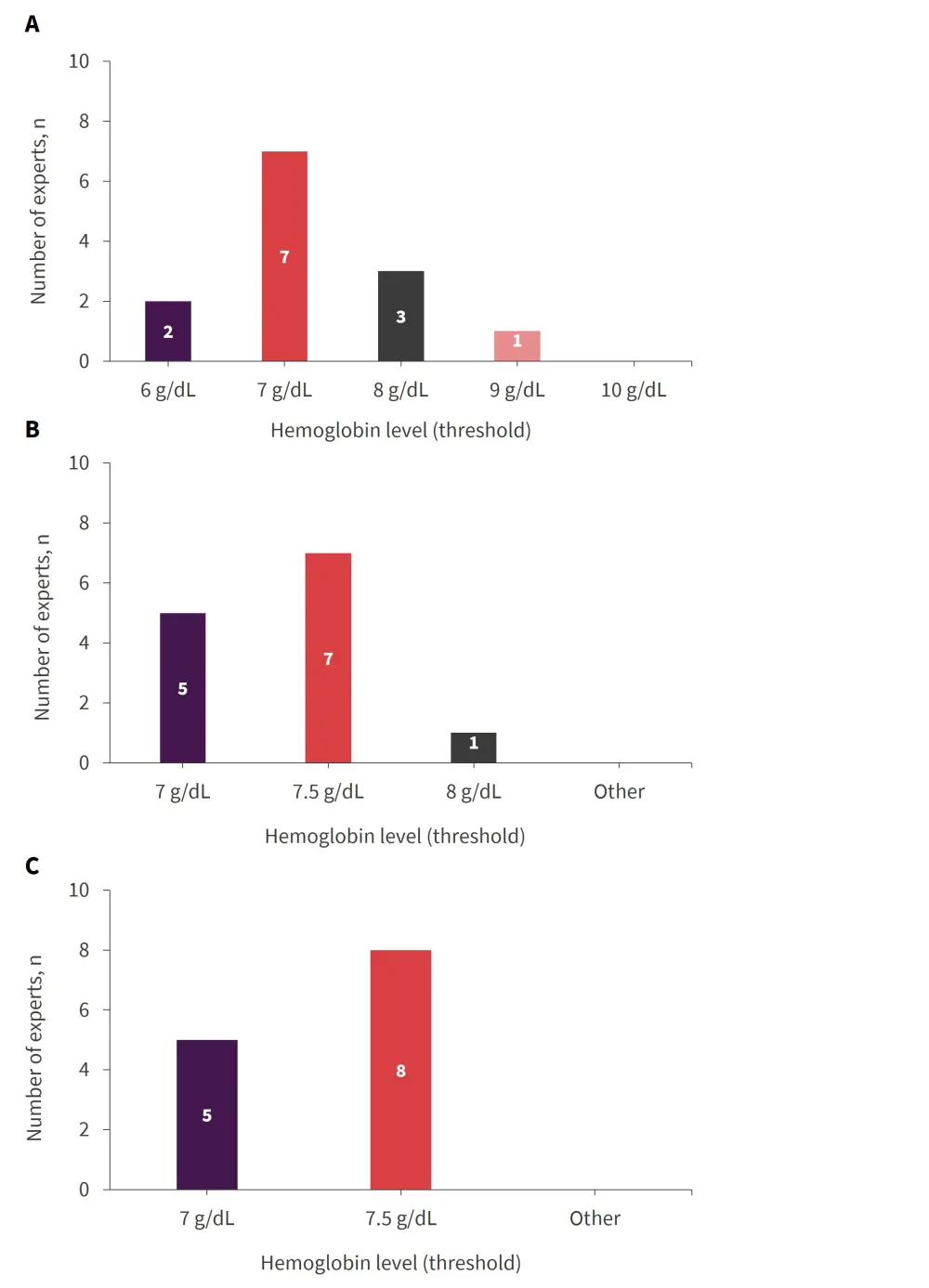
*Adapted from Abel2
Is a peri-transfusion quality-of-life assessment feasible?
Study design
The quality of life of patients was assessed 1 day before, and 7 days after RBC transfusion. All patients were required to be diagnosed with MDS, have a hemoglobin level ≥7.5 g/dL, and show no evidence of chronic heart failure or unstable angina. An assessment with +/− 5 points was considered potentially meaningful.
Results
A total of 38 patients completed the full assessment. The changes in quality-of-life post-transfusion were as follows:
- 35% experienced a clinically significant increase
- 46% experienced no change
- 19% experienced a decrease
The mean increase between assessments was 14 points, while the mean decrease was 7 points. Patients who had a better baseline quality of life were found to have a greater overall increase. The number of RBCs in the 8-week follow-up was also higher in the assessed group compared to the historical control group (p = 0.03). A total of seven patients discussed their assessments with their providers, with three patients reporting that it affected their decision to pursue future transfusions.
Conclusion
A third of the patients experienced a measurable increase in quality of life 1 week after their transfusion. This highlights the potential for some patients to adopt a more limited transfusion schedule without compromising quality of life. Costs of care and hospitalization should ultimately be compared with costs of new treatments potentially able to avoid RBC transfusion dependence, and to reduce further clinical complications.
Your opinion matters
What hemoglobin level would trigger transfusion assessment in your MDS patients?
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

