All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MDS Alliance.
The mds Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mds Hub cannot guarantee the accuracy of translated content. The mds and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MDS content recommended for you
Health-related quality of life profile of newly diagnosed patients with MDS: A real-world study
Context
Health-related quality of life (HRQoL) is an important factor to consider when treating patients with myelodysplastic syndromes (MDS).1 The lack of benchmark data makes it challenging to interpret HRQoL outcomes in patients with MDS and to contextualize individual patient scores.1 Efficace et al.1 recently published a study in Hemasphere assessing HRQoL in newly diagnosed patients with MDS, including establishing European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC QLQ-C30) reference values.
Study design and patient population
The analysis included 927 adult patients with newly diagnosed MDS from a prospective international patient-reported outcome in MDS (PROMYS) observational study (NCT00809575). Patient HRQoL data were assessed at the start of the study using the self-reported EORTC QLQ-C30 (Figure 1).
Figure 1. EORTC QLQ-C30 overview*

EORTC QLQ-C30, European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30; QoL, quality of life.
*Data from Efficace, et al.1
All scale-standardized scores range from 0 to 100. Higher scores indicate better outcomes for the functional scales and global QoL, whereas higher scores for the symptom scale mean more severe symptoms.
Patient characteristics
Overall, 927 patients enrolled between November 2008 and December 2018 across 53 centers. The median age was 73.3 years (interquartile range, 66.0–79.2). The patients were classified according to the International Prognostic Scoring System (IPSS) risk groups (24.4% low; 30.2% intermediate-1; 33.6% intermediate-2; 11.8% high) and the Revised IPSS (IPSS-R) risk groups (13.0% very low; 24.1% low; 21.8% intermediate; 22.9% high; 18.2% very high).
Key findings1
HRQoL by risk categories
HRQoL scores according to the disease-risk categories (lower vs higher) for the functional scales and symptom scales are shown in Figure 2 and Figure 3, respectively.
Figure 2. EORTC QLQ-C30 functional scales and global health status/QoL scores according to IPSS and IPSS-R in newly diagnosed patients with MDS*
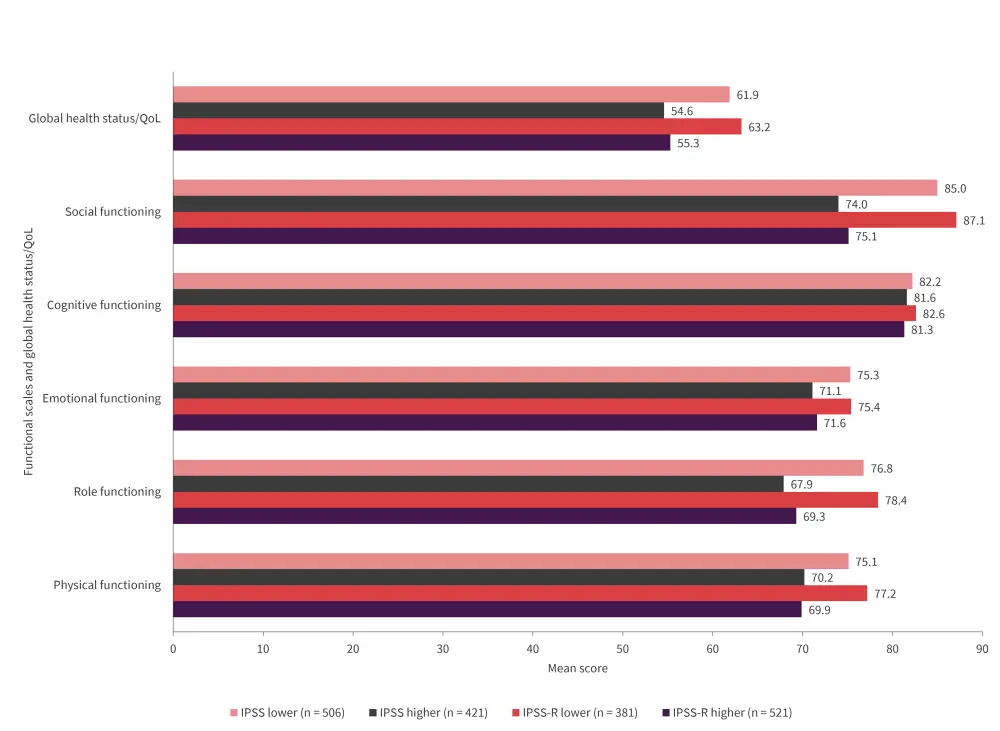
EORTC QLQ-C30, European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core30; IPSS, International Prognostic Scoring System; IPSS-R, Revised IPSS; MDS, myelodysplastic syndromes; QoL, quality of life.
*Data from Efficace, et al.1
Figure 3. EORTC QLQ-C30 symptom scales/items scores according to IPSS and IPSS-R in newly diagnosed patients with MDS*
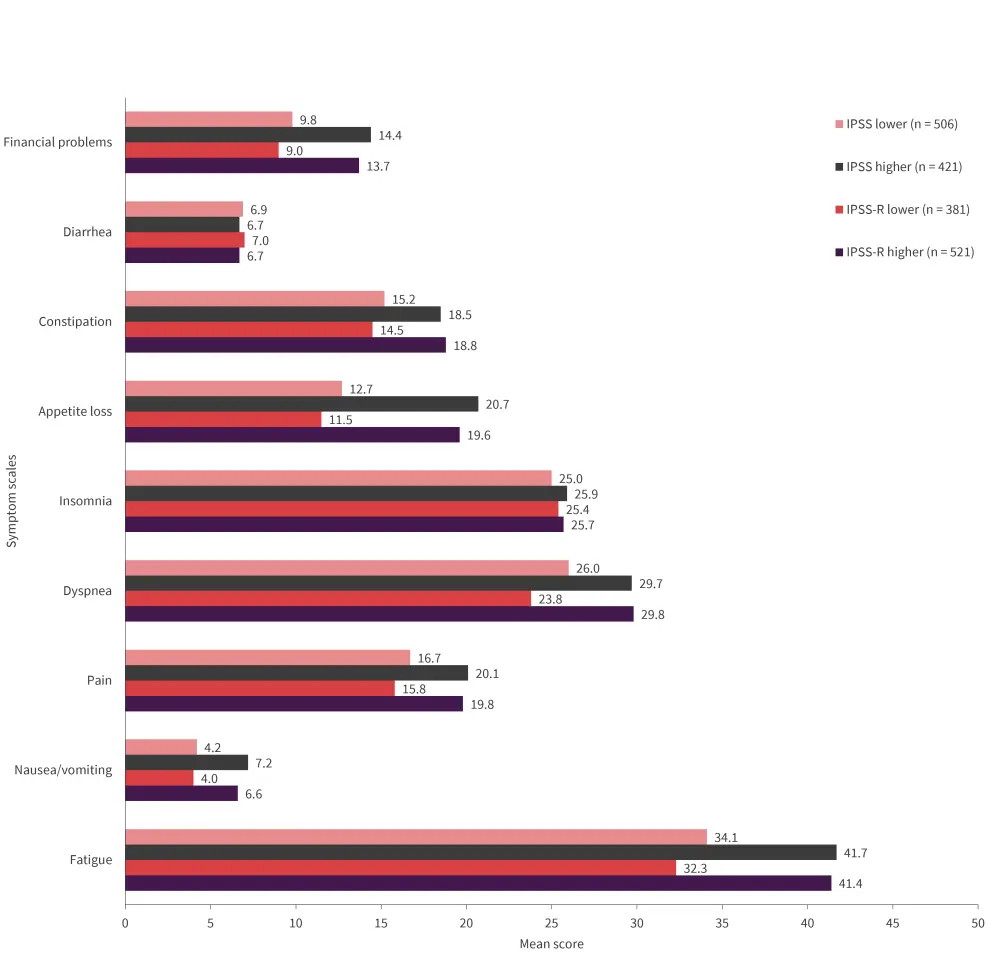
EORTC QLQ-C30, European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core30; IPSS, International Prognostic Scoring System; IPSS-R, Revised IPSS; MDS, myelodysplastic syndromes.
*Data from Efficace, et al.1
HRQoL by age and sex in lower-risk patients
Among men, at least one of the older age groups, when compared with the youngest age group, showed clinically meaningful worse outcomes in 11 scales (physical [PF], role [RF], cognitive [CF], social [SF], QoL, fatigue [FA], pain [PA], appetite loss [AP], dyspnea [DY], insomnia [SL], and constipation [CO]) and better outcomes for one scale (financial problems [FI]).
Among women, at least one of the older age groups, when compared with the youngest age group, showed clinically meaningful worse outcomes in six scales (PF, RF, QoL, FA, AP, and CO). The youngest patients showed worse outcomes in four scales (CF, nausea/vomiting, SL, and FI), and two scales (FA, CO) had a mixed pattern.
HRQoL by age and sex in higher-risk patients
In higher-risk patients, the youngest patients tended to report a lower HRQoL profile compared with older age groups. Men reported overall better HRQoL than women in this group. Among men, at least one of the older age groups, when compared with the youngest age group, showed clinically meaningful better scores in nine scales (PF, RF, CF, SF, FA, DY, SL, AP, FI).
Among women, at least one of the older age groups, when compared with the youngest age group, showed clinically meaningful better scores in six scales (PF, FA, PA, DY, AP, and FI).
Regression models for prediction of EORTC QLQ-C30
These data were used to develop two separate regression models to allow the prediction of EORTC QLQ-C30 scores for patients with either IPSS or IPSS-R risk scores available and with specific distributions of age, sex, and the presence of comorbidity.
Key learnings
The findings from this study could serve as a benchmark in future MDS studies utilizing the EORTC QLQ-C30 questionnaire to enhance the interpretation of any effect on HRQoL.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

