All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MDS Alliance.
The mds Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mds Hub cannot guarantee the accuracy of translated content. The mds and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MDS content recommended for you
Comparison of clinical and genetic features of CCUS and lower-risk MDS
Clonal cytopenia of undetermined significance (CCUS) is a hematologic disorder characterized by persistent cytopenia with genomic aberrations. Despite research demonstrating similarity of CCUS with lower-risk myelodysplastic syndromes (MDS) in the absence of dysplasia and chromosomal aberrations, patients with CCUS do not have access to the same treatment options.
In a recent study published by Eun-Ji Choi and colleagues1 in the British Journal of Haematology, the clinical and molecular characteristics of idiopathic cytopenia of undetermined significance (ICUS), both non-clonal and clonal, were compared in patients with MDS. We summarize key results below.
Methods
Patients with lower-risk MDS (LR-MDS) or ICUS diagnosed between May 2009 and December 2019 at the Asan Medical Center, University of Ulsan, Ulsan, KR, were included for analysis. Inclusion criteria are summarized in Figure 1.
Figure 1. Study design*
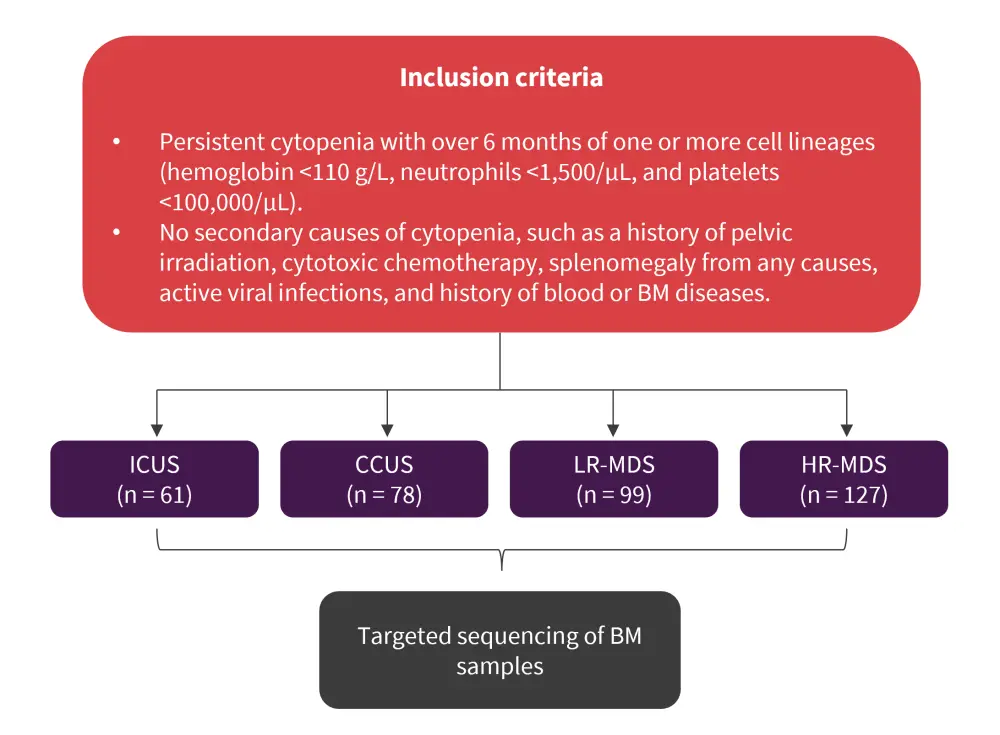
BM, bone marrow; CCUS, clonal cytopenia of undetermined significance; HR-MDS, higher-risk MDS; ICUS, idiopathic cytopenia of undetermined significance; LR-MDS, lower-risk MDS; MDS, myelodysplastic syndromes.
*Adapted from Choi et al.1
Results
Patient characteristics for all subgroups of patients are shown in Table 1.
Table 1. Patient characteristics*
|
ANC, absolute neutrophil count; BM, bone marrow; CCUS, clonal cytopenia of undetermined significance; ESA, erythropoiesis-stimulating agent; Hb, hemoglobin; HR-MDS, higher-risk myelodysplastic syndromes; IPSS-R, revised International Prognostic Scoring System; LR-MDS, lower-risk myelodysplastic syndromes; ncICUS, non-clonal idiopathic cytopenia of undetermined significance; PLT, platelets; RBC, red blood cells; WBC, white blood cells. |
||||
|
Characteristic |
ncICUS |
CCUS |
LR-MDS |
HR-MDS |
|---|---|---|---|---|
|
Female, % |
60.7 |
39.7 |
33.3 |
39.4 |
|
Age, median in years (range) |
52 (19–77) |
65 (19–89) |
59 (19–85) |
61 (18–87) |
|
WBC, × 103/µL, median (range) |
3.4 |
3.4 |
3.2 |
2.9 |
|
ANC, × 103/µL, median (range) |
1,493 |
1,395 |
1,456 |
922 |
|
Hb, g/L, median (range) |
115 |
105 |
90 |
84 |
|
PLT, × 103/µL, median (range) |
96 |
88.5 |
106 |
73 |
|
BM cellularity, median (range) |
30 |
30 |
40 |
50 |
|
BM blast, %, median (range) |
1.0 |
1.2 |
1.4 |
5.2 |
|
IPSS-R karyotype risk, % |
||||
|
Very good |
0 |
9.0 |
6.1 |
0.8 |
|
Good |
96.7 |
79.5 |
80.8 |
33.1 |
|
Intermediate |
0 |
9.90 |
13.1 |
33.9 |
|
Poor |
0 |
0 |
0 |
14.2 |
|
Very poor |
0 |
0 |
0 |
18.1 |
|
Unknown |
1.6 |
2.6 |
0 |
— |
|
IPSS-R, % |
||||
|
Very low |
44.3 |
28.2 |
9.1 |
0 |
|
Low |
45.9 |
59.0 |
69.7 |
0 |
|
Intermediate |
8.2 |
9.0 |
21.2 |
46.5 |
|
High |
0 |
0 |
0 |
29.9 |
|
Very high |
0 |
0 |
0 |
23.6 |
|
Unknown |
1.6 |
3.8 |
0 |
— |
Genetic and clinical features
- Patients with CCUS had lower hemoglobin and higher bone marrow cellularity than patients with LR-MDS
- CCUS and LR-MDS had similar genetic features, and the most frequently mutated genes in both groups were TET2 (23.1%), DNMT3A (20.5%), DDX41 (12.8%), and ASXL1 (7.7%)
- The frequency of SF3B1 mutations was significantly lower in patients with CCUS compared to patients with LR-MDS (2.6% vs 18.2%; p = 0.001)
- The variant allele frequency (VAF) values of U2AF1 (19.6% vs 38.1%; p = 0.075) were lower in patients with CCUS compared to those with LR-MDS
- Patients with higher-risk MDS (HR-MDS) had a significantly higher frequency of mutations in CBL, EZH2, PHF6, and TP53 compared with both CCUS and LR-MDS
Prognostic factors for survival in CCUS
- Despite their older age, overall survival (OS) was superior in patients with non-clonal idiopathic cytopenia of undetermined significance (ncICUS) compared to CCUS, whereas patients with CCUS had a superior OS compared with LR-MDS (Figure 2).
Figure 2. 5-year median OS for all subgroups of patients*
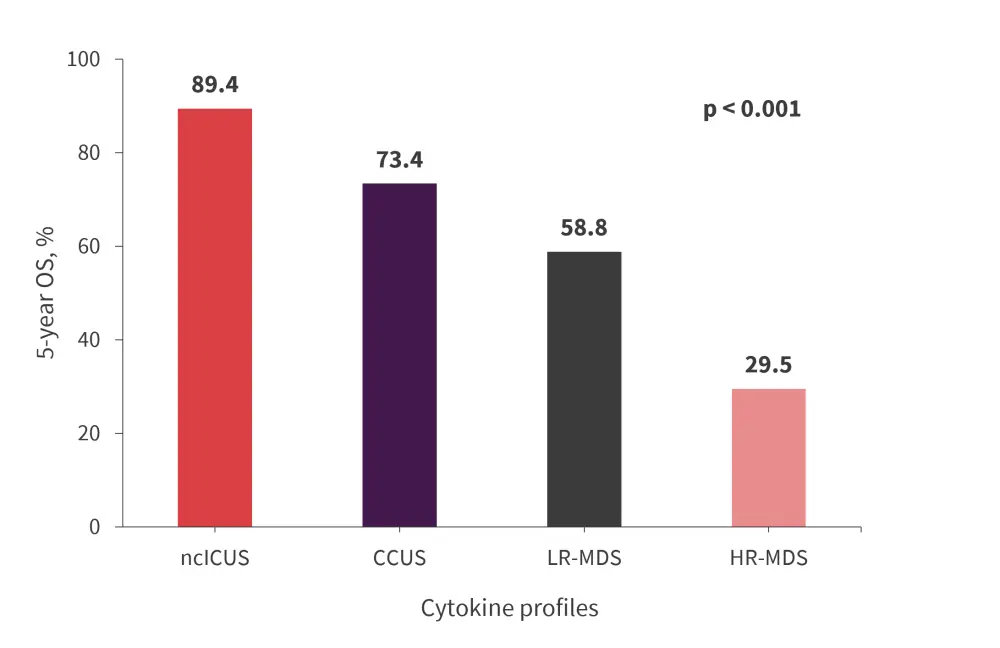
CCUS, clonal cytopenia of undetermined significance; HR-MDS, higher-risk myelodysplastic syndromes; LR-MDS, lower-risk myelodysplastic syndromes; ncICUS, non-clonal idiopathic cytopenia of undetermined significance; OS, overall survival.
*Adapted from Choi et al.1
- A multivariate analysis for survival in CCUS revealed that lower hemoglobin at diagnosis, presence of mutations in DDX41, ETV6, and RUNX1, were significantly associated with worse OS (Table 2).
- Hemoglobin at diagnosis and DDX41 mutations were also significantly associated with worsened progression-free survival (PFS) in CCUS.
Table 2. Multivariate analysis for survival in CCUS*
|
CCUS, clonal cytopenia of undetermined significance; CI, confidence interval; Hb, hemoglobin; HR, hazard ratio; IPSS-R, revised International Prognostic Scoring System; OS, overall survival; PFS, progression-free survival. |
|||||
|
Characteristic |
OS |
PFS |
Prognostic score |
||
|---|---|---|---|---|---|
|
HR (95% CI) |
p value |
HR (95% CI) |
p value |
|
|
|
Hb at diagnosis, g/L |
|||||
|
≥90 |
1 |
0.011 |
1 |
0.008 |
|
|
<90 |
7.39 |
|
7.39 |
|
1 |
|
DDX41 mutation |
|||||
|
Absent |
1 |
0.004 |
|
0.002 |
|
|
Present |
12.22 |
|
10.62 |
|
1 (germline and somatic) |
|
ETV6 mutation |
|||||
|
Absent |
1 |
0.003 |
— |
— |
|
|
Present |
30.68 |
|
— |
— |
2 |
|
RUNX1 mutation |
|||||
|
Absent |
1 |
|
— |
— |
|
|
Present |
7.07 |
0.039 |
— |
— |
1 |
- Notably, patients with CCUS who also harbored these poor-risk prognostic factors had similar or worse OS than patients with LR-MDS
- The authors1 created a scoring system for patients with CCUS who had the above-mentioned adverse prognostic factors, scoring one point for those with hemoglobin <90 g/L, biallelic germline and somatic DDX41 mutation, or RUNX1 mutation, and two points for the presence of ETV6 mutation
- Patients were divided into three risk categories which showed a significant difference in the 5-year OS (Figure 3)
Figure 3. 5-year OS based on prognostic risk score in patients with CCUS*
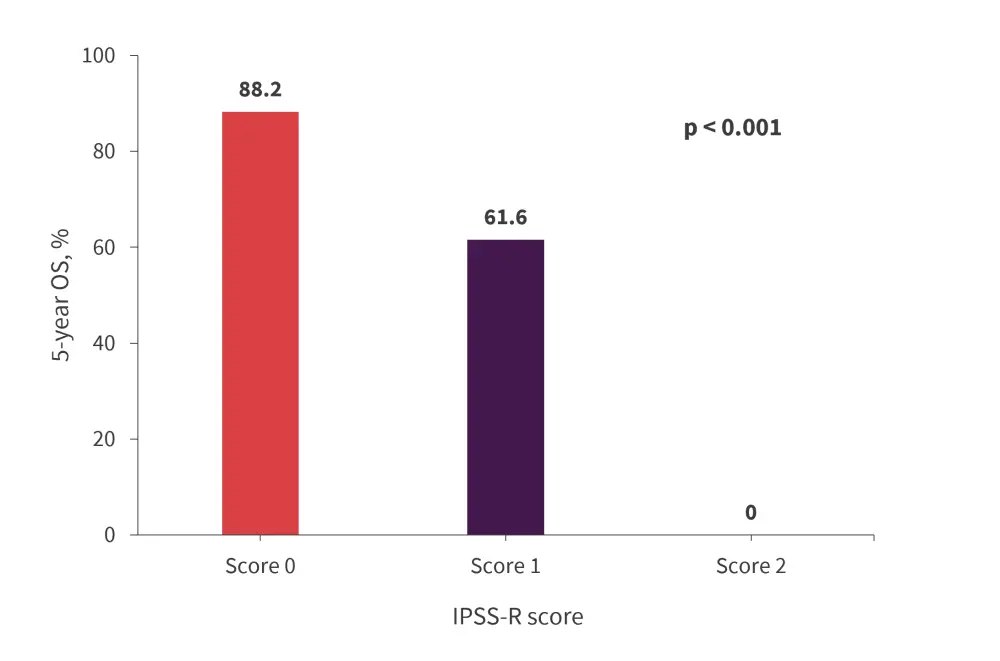
CCUS, clonal cytopenia of undetermined significance; IPSS-R, revised International Prognostic Scoring System; OS, overall survival.
*Adapted from Choi et al.1
Conclusion
The study1 provided evidence for similar survival outcomes and genetic features in patients with CCUS and LR-MDS. This was particularly pronounced in patients with adverse high-risk features, including lower hemoglobin, high mutation numbers and burden, and DDX41 mutations, who achieved similar or slightly worse OS than patients with LR-MDS. As such, CCUS should be treated in a comparable manner with LR-MDS, and patients with high mutation numbers, allele burden, and mutations in genes encoding splicing factors should be closely evaluated.
Study limitations highlighted by the authors, included the small number of patients enrolled which limited evaluation of prognostic factors and mutational patterns. Also, there is a possibility of selection bias due to the data being collected both prospectively and retrospectively.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

